Wear a homemade mask!! plus science summaries and data viz
Published:
You can see previous pandemic blog posts here, here, here, and here. As always, you should take everything you read on the internet with a healthy dose of skepticism, but I try to provide relevant evidence from credible sources.
The CDC has issued guidelines recommending all Americans to wear homemade masks when out in public. This does not mean you should go buy hospital-grade personal protective equipment (PPE). Please save that for the health care workers! But what led to this new recommendation?
I watched an event tonight with NIH Director Dr. Francis Collins hosted by Biologos, and he reiterated that the virus is primarily transmitted via droplets from sneezing and coughing. However, he mentioned unpublished work by an NIH investigator that used laser technology to show that speaking was emitting droplets that could contain viral particles. This is the main argument for why we should be wearing masks out in public now. He reiterated that we’re being asked to wear masks not to protect ourselves, but to protect someone else on the chance that we are infected and don’t know it. Staying 6 feet apart remains a critical part of reducing transmission.
On the other hand, health care workers need masks to protect themselves from infected patients, and that’s where an N95 respirator is key. This naming convention comes from the National Institute for Occupational Safety and Health (NIOSH) air filtration ratings with N meaning “Not resistant to oil” and 95 meaning the respirator has a 95% efficiency for filtering particles of 0.3 micrometers, and a greater than 95% efficiency for particles less than and greater than 0.3 micrometers. Respiratory droplets are 5 to 10 micrometers in size. A study from Korea found the virus to be 0.07-0.09 micrometers in size. Smaller droplets called bioaersols can be produced when we talk and breathe, and these can travel further and stay in the air long. The virus can also be aerosolized during medical procedures like intubation which one reason our health care workers need proper PPE.
The prestigious National Academies of Sciences, Engineering, and Medicine has a Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats. Their communication to the Executive Office of the President laid out the current scientific evidence for viral transmission as of April 1, 2020. Some of the evidence is in pre-prints, these are publications by bonafide scientists that have not be subjected to the usual peer review but allow rapid dissemination of findings. Among the research presented was evidence from Nebraska which detected viral RNA from air collectors greater than 6 feet away from COVID-19 patients. Just because viral RNA is present doesn’t mean the virus would remain infectious, but it does mean particles are likely travelling as bioaerosols. Samples taken from hospitals in Wuhan suggested the virus may be resuspended as an aerosol by PPE removal or cleaning procedures in hospitals, but encouragingly found undetectable or very low concenrations of SARS-CoV-2 aerosols in public locations. The two key sentences of the letter are “Currently available research supports the possibility that SARS-CoV-2 could be spread via bioaerosols generated directly by patients’ exhalation.” and “However, for no respiratory virus is the exact proportion of infections due to air droplet, aerosol, or fomite transmission fully established, and many individual factors and situations may contribute to the importance of each route of transmission.” The scientific evidence laid out in the letter is thought to be the driving force behind the CDC recommendation. Here is a nice piece by NPR on the droplet transmission of the virus.
Transmission by pre-symptomatic cases is another motivator for wearing masks, so you can protect others before you know you’re infectious. A study out of China showed SARS-COV-2 is more efficiently transmitted than SARS-CoV, the virus responsible for the 2003 SARS epidemic, largely through active viral shedding at a time when symptoms are still mild and indicative of an upper respiratory infection (in the throat as opposed to lung).
Another piece of the puzzle is the unknown prevalence of asymptomatic cases. As early as January there were case reports emerging from China of asymptomatic carrier transmission. The journal Nature summarized research in this space as of March 20, 2020. A NEJM correspondence regarding a small sample from China showed an asymptomatic patient had a similar viral load (e.g. amount of virus present) to the symptomatic patients in a nasal and throat swab.
As I highlighted on the March 16, 2020 Update, testing on the Diamond Princess Cruise ship showed 50.5% (320 of 634) of positive cases to be asymptomatic. Statistical modeling allowed researchers to estimate how many were likely to develop symptoms after the time of observation. They estimated that 17.9% (95% confidence interval of 15.5-20.2%) of positive cases were truly asymptomatic.
Widespread testing in Iceland by deCODE genetics was recently published in a non-peer-reviewed pre-print. Since testing capacity is limited in most countries, we generally only know about COVID-19 test results in high-risk populations (e.g. very sick patients in the hospital, health care workers). In Iceland they screened a mostly random sample of the population (N=5,502) and found 0.9% to be positive for COVID-19. 33 of the 50 (66%) with a positive test from the population screening had symptoms meaning 34% were asymptomatic or pre-symptomatic. On the other hand, the targeted screening yielded 10.1% positive of 1,928 (86.4% with symptoms) from the time frame February 1 to March 15 and yielded 13.4% positive of 2,623 (92.6% with symptoms) from the time frame March 16 to March 22.
A French publication, RFI, interviewed an Italian virologist who tested the entire population (N=3,300) of a small town, Vò, in Northern Italy. They found 3% of the population to be positive and the majority did not have symptoms. Unfortunately I haven’t seen data or additional details for this study.
Because the estimate of asymptomatic case prevalence ranges quite a bit, you might be tempted to throw up your hands and believe none of it. In statistics we note limitations to population-specific estimates by reminding readers that each population has its own quirks or the ascertainment of cases in different populations may vary. Despite the estimate’s uncertainty, the findings can still point us to a conclusion that asymptomatic and pre-symptomatic cases can spread the virus. Hence the importance of wearing masks in public! Please read important information from the World Health Organization (WHO) about how to safely put on, wear, and remove a mask is here.
Here are some scientific studies summarized:
A vaccine was tested in mice using microneedle arrays instead of the normal subcutaneous (e.g. under the skin) needle injection. The immune response was found to be stronger with the skin-targeted delivery than the normal injection. The immune system’s response is measured by a technique called ELISA (enzyme-linked immunosorbent assay) which can quantify the amount of antibody present in the blood. They found the mice developed antibody responses specific to SARS-CoV-2 within 2 weeks of immunization. This group was poised to work on the vaccine due to previous work developing a microneedle array vaccine for MERS. In fact, since the viruses are so similar, their longterm evidence of the vaccine’s ability to generate long lasting (> 1 year) antibodies is encouraging that the same will be true for the SARS version. They are hoping to start a phase 1 human clinical trial soon. You can read the scientific paper and the press release from University of Pittsburgh. There are teams all over the world working on potential vaccines. This is good news because we have more chances for one to work, and if multiple work then we can scale up society-wide immunization sooner. The first U.S. phase 1 clinical trial began in mid March for a vaccine made by National Institute of Allergy and Infectious Disease (NIAID) scientists and Moderna. A commentary in The Lancet elaborates on the three imperatives for vaccine development: speed, manufacture and deployment at scale, and global access.
We hear about the respiratory problems of COVID-19 patients, but doctors are also finding cardiovasacular issues. In an investigation published in JAMA Cardiology, scientists in Wuhan retrospectively (e.g. observed after the outbreak) analyzed 187 patients from January 23 to February 23. 27.8% exhibited myocardial injury, which means damage to the heart muscle. This myocardial injury is associated with fatal outcome, as well as cardiac dysfunction and arrhythmias. However, patients with underlying heart disease who do not experience myocardial injury had a relatively favorable outcome. In order of largest to smallest percentage of in-hospital fatalities 1) heart disease + myocardial injury 2) myocardial injury only 3) heart disease without myocardial injury 4) neither heart diseae or myocardial injury (please see Figure 2). There’s a lot of debate regarding the mechanism of action for this damage. Perhaps the virus is infecting the heart and causing damage or maybe the body’s immune system is causing damage. Kaiser Health News, which is an editorially independent program of Kaiser Family Foundation (not associated with health insurer Kaiser Permanente) published an in-depth piece on COVID-19 associated heart damage.
A recent study used a method called cryo-electron microscopy to visualize the interaction of human protein and the SARS-CoV-2 virus. Knowing the structure will be helpful for developing therapeutics. The virus’ spike protein binds to angiotensin-coverting enzyme 2 (ACE2) which is expressed in lung, hence the predominantly respiratory nature of the illness. Because angiotensin-coverting enzyme (ACE) inhibitors are used to treat high blood pressure and heart failure, clinicians wondered how this drug would interact with viral infection. Another study determined that ACE inhibitors (and the broader class of renin-angiotensin-aldosterone system [RAAS] inhibitors) can be continued in COVID-19 patients, although they caution more study is needed in this area. This was all summarized in a blog post by NIH Director Dr. Francis Collins.
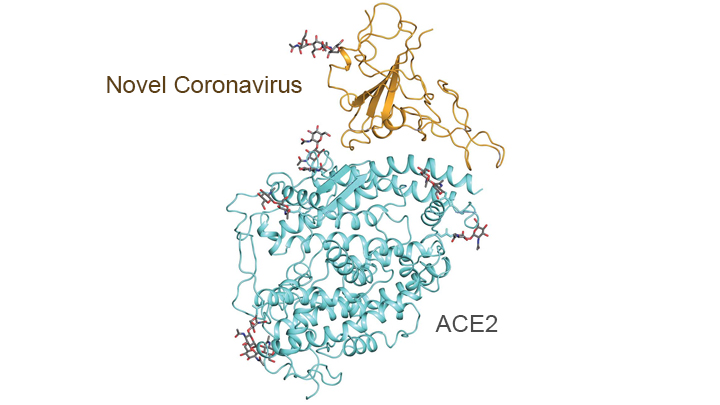 |
Molecular map showing interaction between the spike protein (gold) of the novel coronavirus and the peptidase domain (blue) of human angiotensin-converting enzyme 2 (ACE2). Credit: Adapted from Yan R., Science, 2020 for the NIH Director’s blog.
Here are some epidemiological model updates:
A specific model for North Carolina was created by independent NC epidemiologists and data scientists.
A specific model for Michigan was created by university of Michigan epidemiologists.
The University of Washington’s IHME updated their models on April 5 and they describe these changes transparently and in-depth. State-level hospital use and the impact of social distancing provided a lot more information for parameter estimates. Overall the forecasts are more favorable but the estimates have a larger uncertainty.
Here are some nice illustrated explanations and data visualizations:
Here is a beautiful explanation by a respected science writer, Carl Zimmer. He explains how each of the segments of the viral RNA create proteins that perform specific tasks. The structure of the virus is important to finding drug targets as Dr. Francis Collins highlights in his NIH blog, mentioned above.
Yale created an illustrated scientific summary of how the virus causes COVID-19 symptoms and how it is spread.
A visualization comparing daily COVID-19 deaths to other top causes of death in the U.S.
