Memorial Day during a pandemic
Published:
Today is Memorial Day in the United States, a day when we honor those who lost their lives in service to our country. It is also a day we approach 100,000 COVID-19 deaths in the U.S. Yesterday, the NY Times memorialized just 1% of those deaths starting on the Sunday front page. If we add every U.S. military death from the beginning of the Korean War in 1950 through all wars and conflicts up to today, we arrive at a similar number of 102,483 deaths (Note: this value is based on this table and could be more or less depending on inclusion of MIA or other nuances). In three months we have lost nearly the amount of Americans as the military personnel we’ve lost in 70 years of conflicts. To memorialize the sacrifice of those who gave their lives for the U.S., we should use our hard-fought freedoms responsibly to help our society and economy move forward as safely as possible in the presence of SARS-CoV-2. I acknowledge that the majority of our country is being conscientious and generous in their sacrifices, and I empathize that everyone has their own unique situation, but we are all interconnected in this pandemic. I believe the following are things we can do to live up to the American way our service members fought and died for.
1. Stacking best practices
At the end of April, the dean of the University of Michigan School of Public Health and associate dean of education at UM SPH penned an op-ed regarding stacked best practices as Michigan and the country begin to allow certain businesses to operate again. Drs. Bowman and Kardia wrote: Our research tells us that stacking best practices—with several layers of safeguards to reduce the spread of COVID-19 and lower the risk of another spike in cases and deaths—is necessary to manage this outbreak while re-engaging our economy.
They make an analogy that stacked best practices like mask wearing, hand washing, sneeze guards for cashiers, split work time in cubicle settings are the same as the group of behaviors we engage in around driving: air bags, stop signs, speed limits. You can watch this video which further explains this analogy.
Esteemed physician and writer Dr. Atul Gawande also wrote about a regimen for re-entry. He similarly discusses the “combination therapy” we should embrace upon re-opening just as we use combination therapies for cancer. “Its elements are all familiar: hygiene measures, screening, distancing, and masks. Each has flaws. Skip one, and the treatment won’t work. But, when taken together, and taken seriously, they shut down the virus.”
An Assistant Professor at the Johns Hopkins University Center for Health Security, Dr. Caitlin Rivers, shared a Twitter thread with her thoughts on viral transmission in a more open world. “Our actions, the choices we make, are the front lines. We should stay home when we can, avoid gatherings, wear masks indoors in public, wash hands. This next phase is up to us, and it’s with continued vigilance that we can further slow the virus.”
Several pre-prints have modeled the impact that universal mask wearing can have on the pandemic. Eikenberry et al states, “Despite uncertainty, the potential for benefit, the lack of obvious harm, and the precautionary principle lead us to strongly recommend as close to universal (homemade, unless medical masks can be used without diverting healthcare supply) mask use by the general public as possible.” In Figure 1 of Howard et al we see at 80% adherence and 40% mask efficacy we would reduce the reproduction number to < 1 which is the goal to eventually end viral spread.
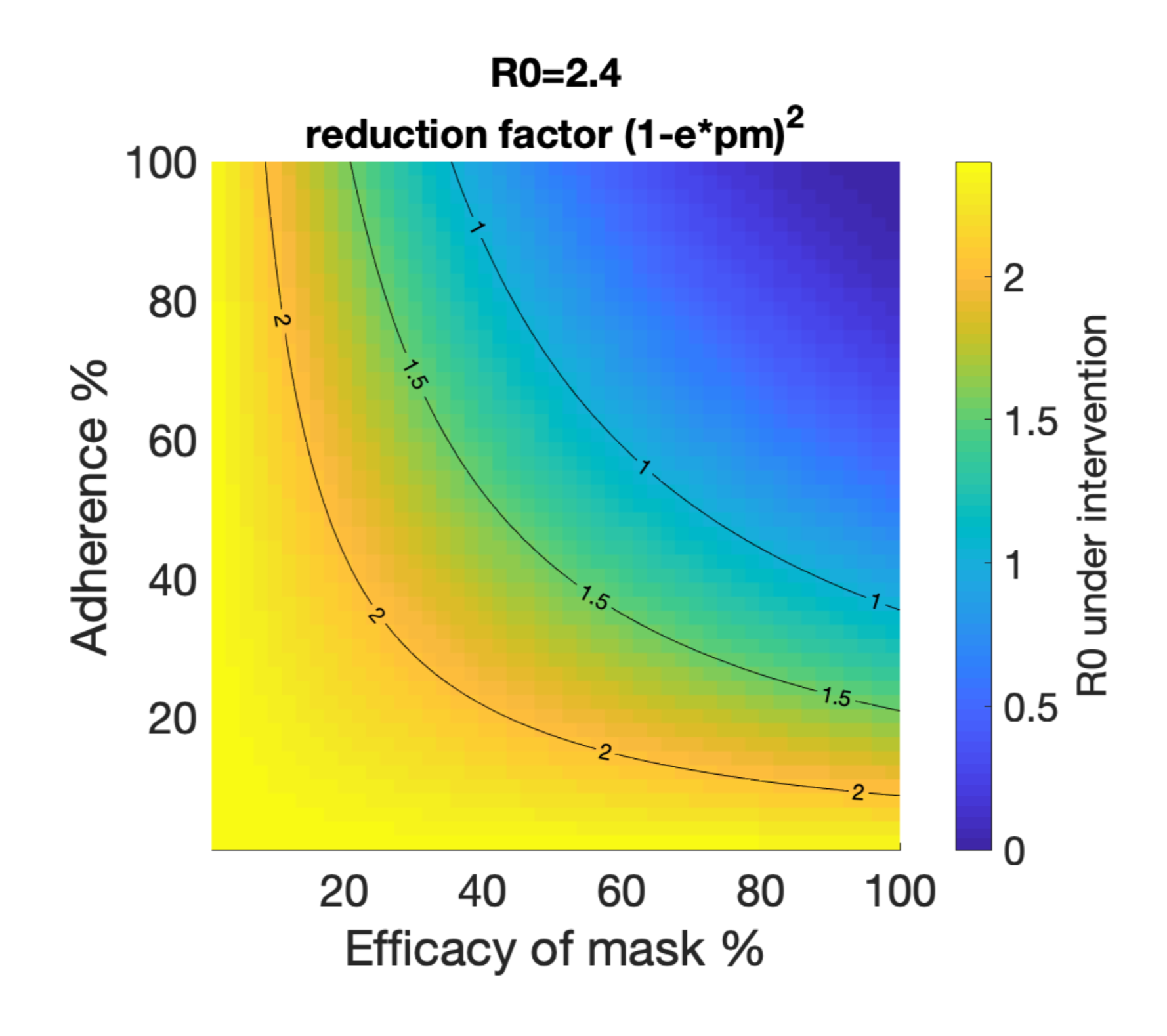
The impact of public mask wearing as modeled in a pre-print by Howard et al. We want to be in the blue.
The purpose of stacking best practices is holistic risk reduction. An epidemiologist at Boston University, Dr. Ellie Murray, suggests considering a COVID-19 contact budget. She and other scientists created an infographic on risk across a variety of settings. You can read more about what experts think of risks across settings here and here. Neurologist and science communicator, Dr. Samantha Yammine summarized a lot of risk reduction resources in an Instagram post. She points out the four dimensions of risk are distance, environment (indoors or outdoors), activity, and time. The two directions we have to consider are risk to our personal health and risk to others.
2. Following public policy
Public policy regarding public health is constantly evolving and sometimes contradictory, especially during an ongoing pandemic. For example, early messaging in the U.S. dissuaded mask usage, but now public policy strongly encourages or mandates masks. You can read more here. Understandably, this is frustrating for the general public. Because knowledge is power, I encourage you to follow the ever-changing public policy landscape as much as you are able. Contact your elected officials to voice your educated opinions too!
The Centers for Disease Control and Prevention (CDC) recently released a lengthy document supporting the President’s plan for re-opening the country. I’ll point you to page 7 which describes thresholds for entering various phases of re-opening. Many states have outlined similar phases. Page 45 has interim guidance for schools and day camps. The CDC also released interim guidance for communities of faith. Because the pandemic has different time lines and magnitudes across the U.S., I encourage you to check the information released by your county and state’s Public Health Departments. Many of these organizations have Facebook pages to communicate with the community.
A new data visualization tool allows simultaneous tracking of social distancing trends, policy decisions, and cumulated COVID-19 cases in the U.S. and in each state. I found this resource thanks to Andy Slavitt’s Twitter and it is hosted by the Surgo Foundation, a self-proclaimed “action tank” working to bring the latest innovations around behavior, tech, and data to global development (I say all this in the effort to consider biases and sources of conflict from the places we get our evidence, read my last post here). As responsible citizens, we have to keep an eye on the complex interplay of viral transmission, interpersonal behavior, and public policy!
3. Educating yourself
If you’re still looking for information about the novel coronavirus, including what it does to lungs and how it infects cells, I suggest the Coronavirus Center at Lifeology. They have several illustrated stories to help kids understand the virus too!
There are a lot of epidemiologists, clinicians, and more sharing their expertise on Twitter. Dr. Angela Rasmussen created a list (made in response to an article highlighting just a few men, but the list stands alone as an incredible source outside of the issue of representation). Dr. Yammine also curated a list of key sources. I’m particularly enjoying threads by Dr. Natalie Dean (@nataliexdean), Dr. Caitlin Rivers (@cmyeaton), and Dr. Zeynep Tufekci (@zeyenp).
Dr. Yammine and infectious disease researcher Laurel Bristow are doing a lot of science communication around the virus on their Instagram accounts. Check their saved stories! They’re doing thorough research to find the evidence behind their explanations, and are also explaining newly emerging research from pre-prints.
Biology professor Dr. Erin Bromage went viral this month with a post about knowing the risks and avoiding them. He has been presenting solid facts for a general audience on his blog.
4. Keeping an eye on the models
The models of COVID-19 mortality are not perfect. They come with uncertainties and predicted ranges that aren’t always reported or explained. They use parameters like case fatality rate, percent of contacts decreased by social distancing, and effective reproductive number which are different across populations and time. As is expected in science, the models are constantly being revised as new estimates for these parameters are available. An ensemble modeling approach, often used for forecasting even outside of disease outbreaks, may be more accurate. As National Public Radio (NPR) reports: “‘Individual models are being changed every week. They’re sensitive to the last observed data in different ways,’ says Reich. But with an ensemble ‘there’s a certain consistency and robustness. You’re not quite, sort of flapping in the wind.’”
Data Scientist Youyang Gu has a COVID-19 model that seems to be even outperforming the COVIDhub Ensemble model. From what I understand, it uses the classic epidemiology SEIR framework with machine learning to estimate the best parameters that go into the model (e.g. what is the reproductive number, Rt, at this time and place). You can see the historical performance for this model and other best-performing US models as compared to the CDC mortalities. I say all this to say, I’ve been intrigued comparing Gu’s models with reopening and without reopening. Please see this Twitter thread for some caveats of the model. Please note that it was recently reported (here and here) that the CDC and several states have been conflating the viral and antibody tests for COVID-19. They’re in the process of disaggregating the counts from the two tests, but this does mean some of the model’s input data is unreliable and unfortunately our estimates are only as good as the data that goes into them.
Imperial College London released a report on May 21, 2020 reporting new state-level tracking of COVID-19. Across the states they estimate the percent of total population likely to have been infected thus far. This ranges from 0.1% in Hawaii (95% confidence interval indicates the truth is likely in the range of 0.0-0.3%) to 16.6% in New York (with 95% confidence interval of 12.8%-21.6%) For several regions they show the reproductive number with respect to interventions such as business closures. In the report’s summary they state: “We predict that deaths over the next two-month period could exceed current cumulative deaths by greater than two-fold, if the relationship between mobility and transmission remains unchanged. Our results suggest that factors modulating transmission such as rapid testing, contact tracing and behavioural precautions are crucial to offset the rise of transmission associated with loosening of social distancing.”
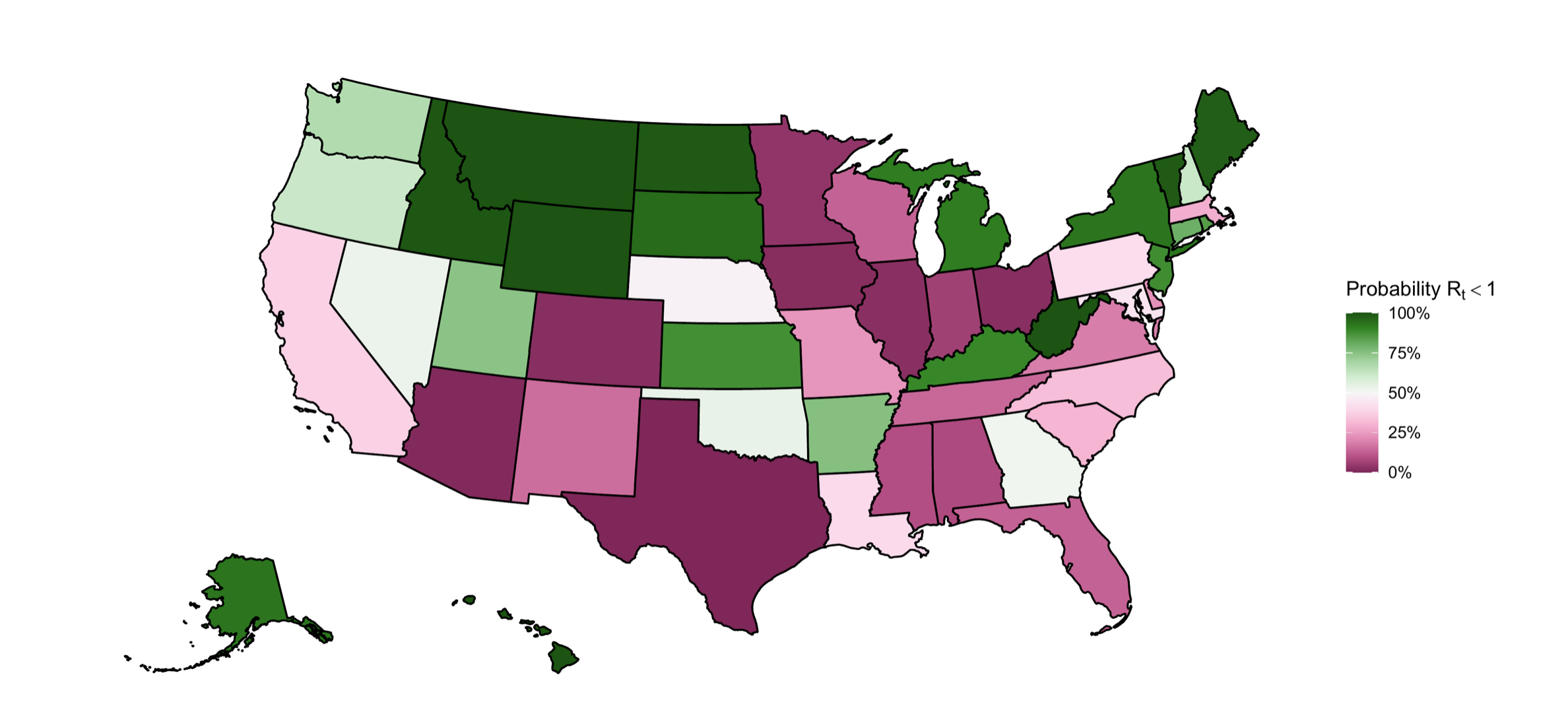
From the latest Imperial College London models, the probability that the reproductive number is <1 (representing epidemic control) for each state as of May 9, 2020. We want to be in the green.
Ultimately, the models are not perfect but they allow us to keep a pulse on potential outcomes given the level of non pharmaceutical interventions (NPI, e.g. social distancing) that we are following. Because of the longer time course for symptoms requiring hospitalizations, we may use models to put the brakes on ourselves before the car starts really rolling down the hill again.
(With regard to the introductory paragraph, I want to acknowledge the loss of life and quality of life to many non-Americans in these conflicts. By using this analogy, I in no way intend to minimize the pain the U.S. military has caused abroad, or even domestically. The ethics of war are important to consider but are not in the scope of this piece. I would also like to acknowledge the history of Memorial Day as it relates to the African American community in Charleston, SC honoring Union soldiers who died in the Civil War.)
